Review of “Changes in Primary Care Physician’s Management of Low Back Pain in a Model of Interprofessional Collaborative Care: An Uncontrolled Before-After Study Chiropractic & Manual Therapies 2013; 21:6 doi:10.1186/2045–709X-21–6”
Interdisciplinary collaborative care between a physician and chiropractor for low back pain patients can create superior patient outcomes and patient satisfaction. The evidence suggests that of the 61% of patients referred for chiropractic services had less neurological deficits, leg pain and 25% fewer physician visits and imaging requests.
This is significant since chronic musculoskeletal conditions can cause disability. Continuity and quality of care provided by the 31% of people with low back or neck pain who seek care from both physicians and chiropractors can be improved. Interprofessional collaborative health care teams delivering coordinated care can create clinically important improvements in patients with musculoskeletal complaints.
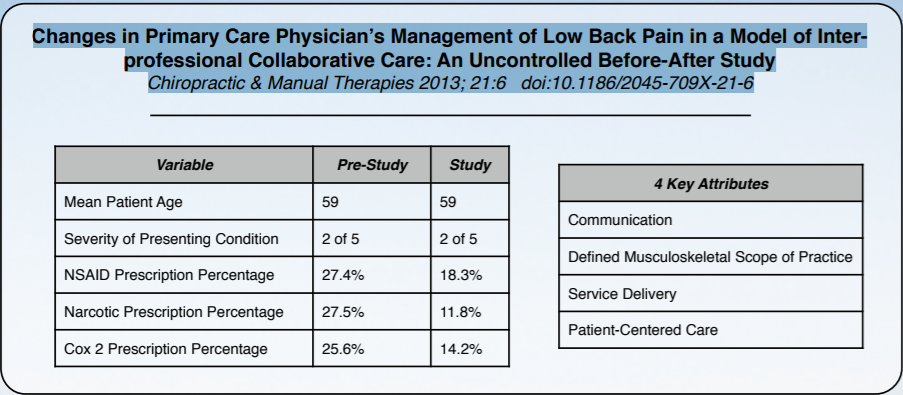
In the pre-study group there were 51 records and in the study group there were 49 available LBP patient records extracted. The primary care physician’s clinical management of patients with low back pain included fewer medications prescribed to study patients compared to pre- study patients, yet the patients had similar pain severity. In a study conducted by Bishop et al. multi-modal based treatments of low back pain showed that the use of narcotic analgesic medications was 78% in the usual care group, compared to 0% in the multi-modal group with similar improvements in bodily pain.
This probably does not come as a surprise, but socioeconomic factors play a significant role in the use of alternative treatments [15,16]. A collaborative model of care with access to no cost alternative therapy appeared to result in less prescription use of medications. This decreased use of medications in patients has been reported previously [19–21] supporting a previous finding that chiropractic care could be used as “a substitute treatment to pain medication”
This is important because approximately one third of patients taking opioids for chronic low back pain are at an increased risk of an adverse drug-drug interaction [22].
The four key attributes of collaborative practice: communication (structured clinical notes, educational sessions, newsletters); defined musculoskeletal scope of practice; service delivery (no patient pay, provider capitated payments, access to diagnostic testing); and patient-centered care (patient choice, focus on prevention/supportive care) [12,13] are the keys to this. These attributes will require behavioral change to enhance the delivery of quality patient- centered care.
Check out my eBook on Chronic Neck Pain.
References
- Hawker G: Epidemiology of arthritis and osteoporosis. In Patterns of Health Care in Ontario: Arthritis and Related Conditions. Edited by Williams J, Badley EM. Toronto: Institute for Clinical Evaluative Sciences; 1998:1–10.
- Von Korff M, Lin EH, Fenton JJ, Saunders K: Frequency and priority of paint patients’ health care use. Clin J Pain 2007, 23:400–408.
- Côté P, Cassidy JD, Carroll L: The treatment of neck and back pain: Who seeks care? Who goes where? Med Care 2001, 39:956–967.
- Hurwitz EL, Chiang L: A comparative analysis of chiropractic and general practitioner patients in North America: findings from the joint Canada/ United States survey of health, 2002–03. BMC Health Serv Res 2006, 6:49. http://www.biomedcentral.com/1472-6963/6/49.
- Mainous AG 3rd, Gill JM, Zoller JS, Wolman MG: Fragmentation of patient care between chiropractors and family physicians. Arc Fam Med 2000, 9:446–450.
- Greene BR, Smith M, Allareddy V, Haas M: Referral patterns and attitudes of primary care physicians towards chiropractors. BMC Complement Altern Med 2006, 6:5. http://www.biomedcentral.com/1472-6882/6/5.
- Garner MJ, Birmingham M, Aker P, Moher D, Balon J, Keenan D, Manga P: Developing integrative primary healthcare delivery: adding a chiropractor to the team. Explore 2008, 4:18–24.
- Maddison P, Jones J, Breslin A, Barton C, Fleur J, Lewis R, McSweeney L, Norgain C, Smith S, Thomas C, Tillson C: Improved access and trageting of musculoskeletal services in northwest Wales: trageted early access to musculoskeletal services (TEAMS) programme. BMJ 2008, 329:1325–1327.
Originally published on Medium